By Renfrew’s PT Team

Intoeing Quick Facts
- Intoeing (or “pigeon toeing”) is defined as the rotational variation of the lower limb where the feet or toes point toward the midline during standing or walking.
- Intoeing is a common anatomical finding in young children.
- In most cases, intoeing is a normal variation of development, is asymptomatic, and does not require intervention.
- Persistent intoeing often does not impact function.
- There is a small subset of children for whom intoeing is a sign of an underlying health condition or who will require specialized intervention.
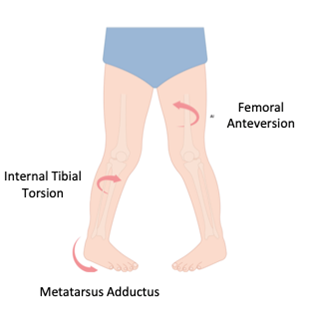
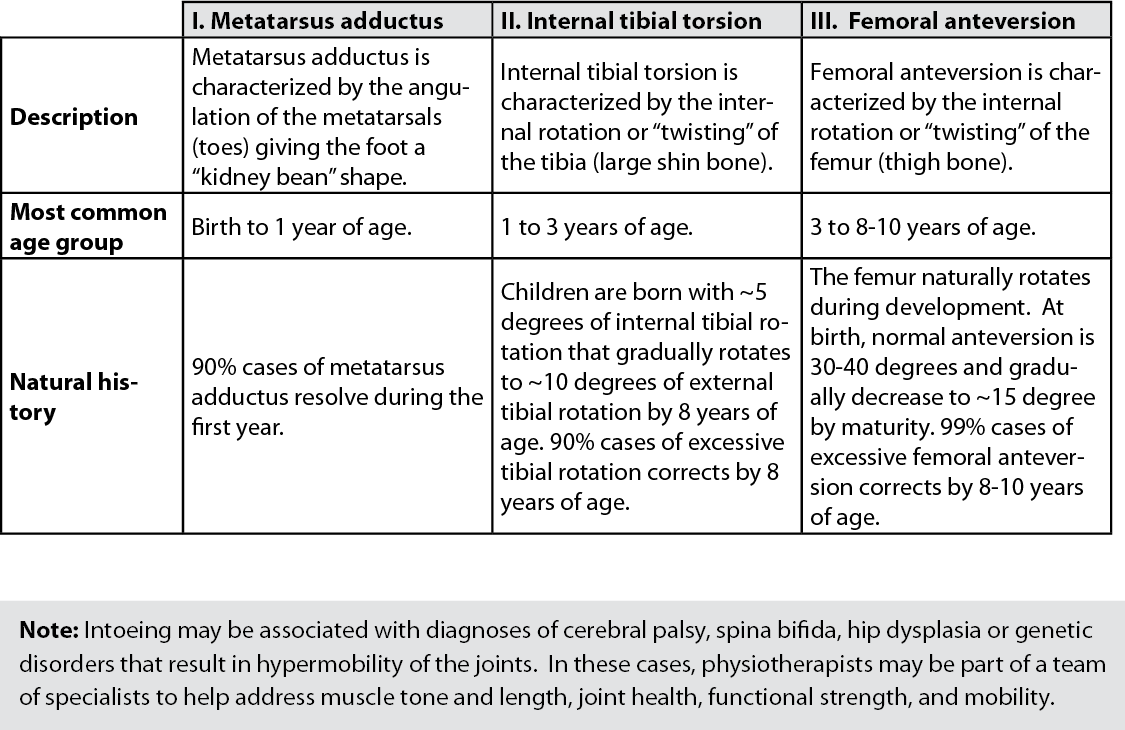
Common Causes of Intoeing
Intoeing is caused by internal rotation at any part of the lower limb. There are three common causes of lower limb rotation and each is more prevalent at different ages.
To Treat or Not to Treat?
- Intoeing typically resolves spontaneously without treatment.
- Evidence suggests that orthotics (i.e., braces or splints), specialized footwear, and stretches/exercises do not affect natural history or help resolve intoeing faster.
- When it persists, intoeing may not impair function or cause adverse outcomes in older children and adults.
- Talk to your physiotherapist or family physician with concerns of any of the following (related to intoeing):
- The child complains of hip, knee, or foot pain with or without limping.
- There is unilateral or asymmetric intoeing.
- There are sudden changes in foot of ankle positioning.
- The child experiences daily recurrent trips or falls.
- The child has a history of abnormal birth or development.
- Intoeing affects the child’s function or gross motor development (e.g. balance or coordination impairments, hip or lower strength weakness, difficulty keeping up with peers, or activity limitations).
- The child is older than ~10 years of age with significant intoeing.
The Role of a Community Physiotherapist
- Complete screen or assessment to determine if intoeing is adversely affecting the child’s function or ability to attain age-appropriate gross motor skills.
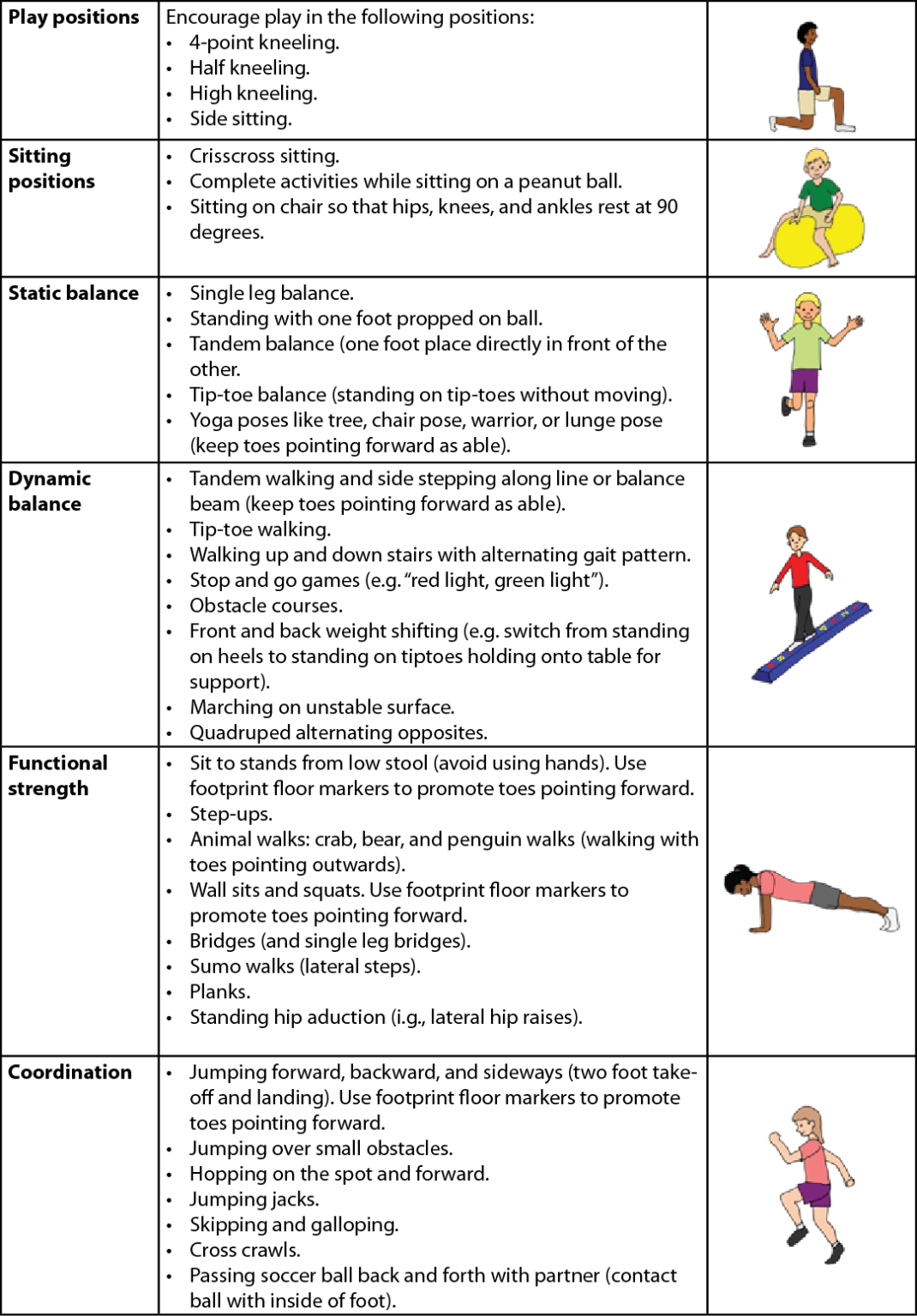
- If indicated, may develop an exercise program to promote the development of gross motor skills (see example below).
- Provide education about sitting, sleeping, and play positions that support healthy development and posture.
- Provide parent and caregiver education about children’s physical and gross motor development.
References
Berry, K. (2018). Evidence-based management of in-toing in children. Clinical Pediatrics, 57(11), 1261-1265.
Cao, L. (2022). When to be concerned about abnormal gait: toe walking, in-toeing, out-toeing, bowlegs, and knock knees. Pediatric Analogue, 51(9), 340-345
Davis, L., & Nativio, D. (2018). Addressing pediatric intoeing in primary care. The Nurse Practitioner, 43(7), 31-35.
Jones, S., Khandekar, S., & Tolessa E. (2013). Normal variants of the lower limbs in pediatric orthopedics. Internal Journal of Clinical Medicine, 4(7B), 12-17.
Rosenfeld, S. (2020, November). Approach to the child with in-toing. UpToDate. https://www.uptodate.com/contents/approach-to-the-child-with-in-toeing.
Sielatycki, J., Hennrikus, W., Swenson, R., Fanelli, M., Reighard, C., & Hamp, J. (2016). In-toeing is often a primary care orthopedic condition. The Journal of Pediatrics, 117, 297-301.
Uden, H., & Kumar, S. (2012). Non-surgical management of a pediatric “intoed” gait pattern- a systematic review of the current best evidence. Journal of Multidisciplinary Healthcare, 5, 27-35.
Exercise Ideas