Hip surveillance is a fancy way of saying hip checkups! It’s the process of monitoring and detecting important early indicators of hip health, especially for children with cerebral palsy (CP). The hip surveillance process monitors for:
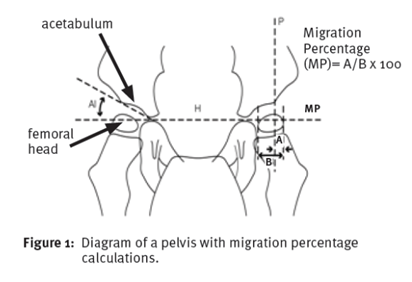
- Hip displacement- The hip bone (femoral head) is shifted to the side (laterally) out of the hip socket (acetabulum) and is measured using a migration percentage (MP) for severity.
- Hip subluxation- The hip bone is partially out of place under the hip socket.
- Hip dislocation- The hip bone is completely displaced from the hip socket

Why is Hip Surveillance Important?
Children with CP have an increased likelihood of hip displacement. Hip displacement, subluxation and dislocation can lead to pain, reduced function and may decrease quality of life. Monitoring early for hip displacement enables the appropriate referral process, can help improve long term hip outcomes, delay surgery as well as best inform hip health management plans.
Surveillance Assessment
Hip surveillance involves a multi-step process for every child with CP and consists of both clinical assessment and radiographic (X-ray) examination. Surveillance is ideally started by 2 years of age for children with a diagnosis of CP or suspected CP.
Hip surveillance frequency varies and is based on a child’s age, GMFCS level, and gait style.
In Calgary, your child with cerebral palsy will likely be followed by the Neuromotor Team at Alberta Children’s Hospital and they will be the main source of education regarding all things hip surveillance.
Did you know? Gross Motor Function Classification System (GMFCS) is a 5-level classification system that describes the gross motor function of children with CP based on their self-initiated movement.
Activities that Promote Hip Health
- All activities that promote weight bearing through the hip joint (e.g., four-point positioning, crawling, high kneeling, assisted standing, walking).
- Prolonged standing in a standing frame is a very important part of hip health for most children with CP.*
- Activities that promote hip and glute strength (e.g., bridging, high kneeling, floor to stand transitions, weight shifting and single leg standing, walking).
- Activities that promote hip range of motion (e.g., positioning and frequent changes in positioning, stretching, regular movement).
- Proper positioning to promote healthy hips and prevent hip subluxation progression (e.g., hip abduction to promote hip joint articulation)


*For children who are not currently able to stand independently, standing in a standing frame is often the best way to promote safe lower limb weight bearing. It is important to note that supported standing in a standing frame should not be substituted for walkers as they each have their own purpose, and children should have access to both (as deemed appropriate by your child’s physiotherapist). Evidence suggests that many of these benefits are achieved when children stand for 45-60 minutes, 5 days a week. *
Please reach out to your child’s physiotherapist or physician with any questions related to hip surveillance and activities to encourage hip development.
References:
AACPDM Guidelines: Hip Surveillance in Cerebral Palsy | AACPDM – American Academy for Cerebral Palsy and Developmental Medicine
Statewide hip surveillance program fact sheet | Children’s Health Queensland
https://pubmed.ncbi.nlm.nih.gov/23797394/
Pelig G, Smith B and Glickman L. Systematic review and evidence-based clinical recommendations for dosing of pediatric supported standing programs. Pediatr Phys Ther. 2013;25(3):232-47.

